Neuroblastoma IV, N-Myc amplification,
Kim's daily history
This page is best read from bottom to top.
The below period is 15 July 2011 at the bottom to 10 April 2012 at the top of the page.
After April 2012 until now...
Kim is now doing good and since had three colds which she overcame all by herself. Her immune system has picked up and she is now learning how to be a normal child. After the first chemo treatment her personality changed. We thought her to be a sweet and timid little baby, well she changed into an outgoing, smart, brave and exuberant little girl. And this one really has no fear of needles!
Of course the risk of a relapse (return of the cancer) is still high. There is currently no science that could tell us what the future will bring or how likely things will go. During Kim's ordeal we have all learned to live a life from day to day and stay happy and positive. Whatever happens, tomorrow will be another day of sunshine. In fact, the sun always shines, even at night or behind the clouds.
Kim is being regularly tested (MIBG, CAT scans, blood and urine tests) to see if there is a relapse. This is done monthly, then increased to every three months, then every six, then every year until....???
Kim did have some slight hearing loss. One of the possible side effect of the chemos. A hearing aid is considered. As the loss is borderline first we try without. So far so good. There are to date no other obvious side effects. Even if they come due time that's normal and as the oncologist was correct to say.. "a small price" in comparison..
10 April 2012 - NOW
Lots of notes/records still to transcribe and add to this website..
04 April 2012, Wednesday
Discharged with pump of Aldesleukin. (next day pump battery low, another trip)
13:30, arrived home
Discharge medications:
Paracetamol 240mg/5ml 3.1ml
Phenergan 5mg/5ml 1.5ml
Bactrim 4ml BD Fri/Sat/Sun
At home over next few days occasional vomiting.
03 April 2012, Tuesday
Weight 11.2kg
Height 86.5cm
11:00, oncologist says Kim is doing quite well.
16:30, Phynagen 3mg and Panadol 100mg every 4hr, ondansetron 2mg every 6hrs.
17:30, Aldesleukin 1.56 MIU in 24ml 5%Glu with Albumin 0.1% for intravenous infusion 1ml/hr (6.24 MIU in 96ml supplied).
23 March 2012, Friday
Last dose of the Sagramostin.
17 March 2012, Saturday
11:30 discharged home.
16 March 2012, Friday
14:00, CH14:18 Monoclonal Antibody, 12.5mg in 100ml sodium-chloride 0.9%, 5ml/hr.
Diarrhoea, morphine boluses given.
15 March 2012, Thursday
14:00, CH14:18 Monoclonal Antibody, 12.5mg in 100ml sodium-chloride 0.9%, 10ml/hr.
Diarrhoea, morphine boluses given.
14 March 2012, Wednesday
Weight 12.0kg (probably lots of fluids, rather than meat on the bone)
Lots of medication to handle her side effects and pain. Kim is much better controlled today. Her heart rate is around 160bpm otherwise she looks fine, not crying or agitation.
20:00, Kim starts to get agitated (side effect of medications).
13 March 2012, Tuesday
weight 11.9kg
CH14:18 Monoclonal Antibody, 12.5mg in 100ml sodium-chloride 0.9%, 5ml/hr. Plenty of other medications and fluids to relief side effects.
16:30, Kim is doing badly, she is very ill. Plenty of Morphine boluses given.
10 March 2012, Saturday
Start of the trial.
Sargramostim 12 micrograms/0.5ml, one injection daily for next 14 days.
02 March 2012, Friday
10:00, discussed all the latest test results with Oncologist. HURRAY!!!! We are all very happy with Kim doing well, or should we say cancer having died well. There are no traces of the cancer. Of course it takes only one tiny cancer cell to start everything again. So now on to the next phase. The trial with CH14:18 Monoclonal Antibody. This will increase her own body defences against any possible recurrence/relapse of the cancer cells.
29 February 2012, Wednesday
MIBG at Peter Mac.
28 February 2012, Tuesday
11:00, CT (CAT) scan.
11:45, MIBG
22 February 2012, Wednesday
12:50, MRI of Abdomen and Pelvis and Bone Marrow Aspiration.
14:50, Kim wakes up from her sedation.
Weight 10.8kg
Neutrophils 1.4
HB 101
WBC 2.6
Plt 60
04 February 2012 - 21 February 2012
Kim her weight stays stable, blood counts very very slowly improving. Now and then vomits. But good mood and happy girl.
03 February 2012, Friday
Weight 10.6kg
Height 85cm
10:50, Kim is given another platelet transfusion, 110ml.
11:30, Kim is having an allergic reaction, transfusion is stopped. She is given Phenagen through iv.
12:30, platelet transfusion restarted.
30 January 2012 - 02 February 2012
Daily trip to Peter Mac for radio therapy.
23 January 2012 - 27 January 2012
Daily trip to Peter Mac for radio therapy. Kim starts vomiting. during the weekend after.
17 January 2012 - 20 January 2012
Daily trip to Peter Mac (Peter MacCallum Cancer Centre) for radio therapy (21.6 gray). Done on outpatient basis. These are long stressful days as the traffic makes these long journeys. Mama just got her learners permit (driving license) and finds it even more stressful.
09 January 2012 - 16 January 2012
Weight stays at 10.7kg.
Height, growth to 84.2cm
Blood counts not great but slowly improving (as expected says oncologist)
08 January 2012, Sunday
Kim ate 4 dumplings at dinner time. (Chinese dumplings)
07 January 2012, Saturday
Appetite is improving.
06 January 2012, Friday
Weight 10.8kg
Height 83.2cm
Neutrophils 2.0
HB 89
Plt 22
WBC 4.5
She is slowly improving.
03 January 2012, Tuesday
Weight 10.8kg
Oncologist orders another transfusion of platelets, 100ml
02 January 2012, Monday
Kim is lethargic today. She asks to be carried all the time. Looks sleepy, down. We are all worried about her. We give her extra fluids through NG tube. Wishing her better tomorrow. We all love you Kim, very much!
31 December 2011 / 01 January 2012
Happy New Year Everyone!
Mama writes "2011 is a difficult year for all of us. Kim got diagnosed and received intensive treatment since July. The good things are her responding so well to the treatment. We enjoy having so many nice nurses, doctors, team members and friends around us. They truly support our family. 2012 will be a much better year.
Still vomiting. every so often.
30 December 2011, Friday
11:00, CT (CAT) scan at Peter Mac in preparation for radiation therapy. Advised radio therapy to start 17 Jan 2012.
29 December 2011, Thursday
Weight 10.8kg, height 83.2cm
12:20, Back in hospital, oncologist orders platelets transition 100ml.
Neutrophils 3.04
HB 124
WBC 7.8
Plt 21.
27 December 2011, Tuesday
Kim doing well, but we are still a bit worried as the last two weeks were up and down. Still oncologist discharges Kim.
12:00 arrive home with lots of medications to give her. She still vomits now and then.
26 December 2011, Monday
Vomited and pulled out NG tube. Very sad as it is very uncomfortable to put the NG tube in.
In general doing well. Some friends came to visit, but they don't have access to isolation ward so met in parent/break room.
25 December 2011, Sunday
Kim took a bite of a biscuit. She is getting up and Santa Claus came by and gave lots of presents.
Medications are less and less.
19-24 December 2011
These are long and tough days. Too many medications and too much happening to keep notes. Kim her condition is going up and down.
18 December 2011, Sunday
Pain team review medication. Ketamin, Heparin and Morphine adjusted a few times to find best balance.
17 December 2011, Saturday
Added glucose through iv
Lots of morphine to handle the pain. Drowsy and high Kim, still considerate and sweet as ever. I know I would complain much more... Tough little positive and caring girl.
vomiting. and diarrhoea...
these days long lists of medications.
16 December 2011, Friday
Weight 11.3kg (slowly loosing weight)
vomiting. and diarrhoea...
Bonus morphine shots given (in addition to regular morphine drip)
19:40, Temperature up to 38°C
15 December 2011, Thursday
Weight 11.6kg
04:45 vomiting.
Morphine increased, also a few bolus given.
Already the last few days Kim is not so cheerful anymore. Tired, sometimes giving up and just letting go.
14 December 2011, Wednesday
Weight 11.8kg
05:10 vomiting.
Morphine given to relief the pain from the chemos.
GCSF
13 December 2011, Tuesday
Weight 11.3kg
GCSF
15:50, vomiting.
17:00, vomiting.
Plenty of other medications.
20:00, NG feed started at 30ml/hr
12 December 2011, Monday
weight 11.7kg
10:00, Methylprednisolone
11:00, Promethazine
11:40 vomiting.
12:46, receiving stem cell transplant
13:15, completed stem cell transplant, 86.7ml.
11 December 2011, Sunday
Weight 10.7kg
09:30 vomited. 150 ml fluid intake
18:00, Day 7 of high dose of chemo, Clonazepam. 200ml fluid intake.
10 December 2011, Saturday
Day 6 of high dose of chemo, Melphalan.
Some of the Consolidation Medications these days:
Clonazepam 0.2mg iv Q6H (anti-seizure) 6-12
Fluconacole 50mg daily 20:00 (anti-fungal)
Aciclovir 200mg TDS (anti-viral)
Nystatin 2ml Q2D
Cotrimoxazole 25mg BD (Bactrim)
Heparin 1000 unit through iv daily
Ondansetron 2mg oral or iv 6-8H
Busulphan 12mg iv 6/24 (chemo)
Melphalan 67mg iv once (chemo)
Lactulose 5ml BD Prn
Domperidone 2-4mg 6H Prn.
09 December 2011, Friday
09:00, Day 5 of high dose of chemo, Busulphan.
Weight 11.2kg.
08 December 2011, Thursday
Day 4 of high dose of chemo, Busulphan. NG feed 400ml overnight.
07 December 2011, Wednesday
Weight 11.3kg
Day 3 of high dose of chemo, Busulphan. Some change in medication due to her behaviour. It seems to have a better effect, Kim is calmer. NG feed of 400ml overnight, for the rest she does not eat much. Maybe one nibble here or there..
06 December 2011, Tuesday
Weight 11.3kg
Day 2 of high dose of chemo Busulphan, plus plenty of medications again. Kim is still behaving high and low. She got four times diarrhoea.
05 December 2011, Monday (Sinterklaas)
Day 1 of high dose of chemo, Busulphan. With a long list of medications to keep side effects under control. Kim became very moody, over-active, crying a lot, due to medications. But she did have good appetite. In addition 400ml through NG overnight.
04 December 2011, Sunday
Weight 10.7kg
Admitted to isolation ward for high dose of chemo starting tomorrow. Plenty of medication to prepare her.
02 December 2011, Friday
10:00, GCSF
14:50 MIBG scan
01 December 2011, Thursday
14:00, CT (CAT) scan.
27 November 2011, Sunday
Kim is not eating.
26 November 2011, Saturday
Kim gets a platelet transfusion of 100ml
Kim is not eating at all now. Mama is sick and Oma sleeps with Kim.
25 November 2011, Friday
Kim is not eating that well.
10:20, Oncologist reviews Kim and is happy to continue.
Neutrophils 1.34
WBC 2.4
HB 94
Plt 25 (very low)
24 November 2011, Thursday
12:25, GCSF
23 November 2011, Wednesday
07:00, NG stopped, total 375ml.
10:00, Peter Mac (Peter MacCallum Cancer Centre) to review Kim for upcoming radiation.
13:50, GCSF
22 November 2011, Tuesday
Oncologist is happy with how Kim is coping these difficult days.
Bloods are OK.
Hickman dressing cleaned/changed.
16:00, GCSF
NG feed total 375ml
21 November 2011, Monday
07:00, NG stopped.
13:00, GCSF
20 November 2011, Sunday
08:30, NG finished, she had a total of 380ml.
11:25, Vomiting. after medications and flush.
13:50, GCSF
22:30, NG feed at 45ml/hr
19 November 2011, Saturday
05:00, NG feed finished.
NG tube is also handy to give her the oral medications she needs. Slowly flush with 20ml of water afterwards.
14:00, GCSF
15:00, white radish juiced and 20ml pushed through the NG tube. White radish is said to have anti cancer cell attributes. Flushed with 10ml of spring water. (important not to get the Nasal Gastric tube congested with sticky medicine or food stuffs, always flush).
21:00, NG started 35 ml/hr. We are slowly increasing feed so that she can get used to it. Kim does not eat well during the day and this is a life saver. Alternative would be fluids through iv in hospital. Home is better.
18 November 2011, Friday
Weight 9.8kg (loosing weight)
Height 83.5cm
Neutrophils 12 (very good)
Oncologist says it is time for NG tube. Nastral Gastric tube goes through the nose into the stomach. This way she can receive fluid nutrition. A little pump is attached that slowly drips this all in one fluid food into her stomach.
16:00, GCSF
21:15, first NG feed start at 25ml/hr (while she sleeps).
17 November 2011, Thursday
12:20, GCSF
16 November 2011, Wednesday
Kim doesn't eat good these days.
12:30, GCSF
15 November 2011, Tuesday
Kim gets some glucose through iv.
14:00, Hickman dressing cleaned/replaced.
16:00, arrive home.
14 November 2011, Monday
17:00, vomits.
13 November 2011, Sunday
09:30 vomits
14:15, 3rd day of 5th chemo cycle.
12 November 2011, Saturday
14:15, 2nd day of 5th chemo cycle
Weight 11kg
11 November 2011, Friday
07:50, arrive hospital.
Weight 10.38kg
Neutrophils 0.86
WBC 2.1
HB 114
Plt 235
14:15, start 5th cycle of chemo.
07 November 2011, Monday
14:55, Hickman dressing cleaned/replaced.
Neutrophils 0.56 (good, coming back up)
04 November 2011, Friday
Oncologist says white blood cells and Neutrophils still low, but also expected. Otherwise doing well.
Weight 10kg
Neutrophils 0.27
WBC 0.9
HB 115
Plt 173.
02 November 2011, Wednesday
08:10, GFR test at Nuclear Medicine.
09:15, contrast fluid injected.
10:45, 1st blood
12:20, 2nd blood, discharged.
14:20, arrived home.
Neutrophils 0.23
WBC 0.7
HB 111
Plt 146.
31 October 2011, Monday
Kim is coughing more and more.
28 October 2011, Friday
Kim is doing OK and seems stable. Discharged.
17:00, arrive home.
Augmentin 2.5ml BD for 3 days.
26 October 2011, Wednesday
Temperature around 37.8°C most of the day. Kim is lethargic. Surgical team comes to check. Maybe it is a virus, they do not think it is a wound infection.
19:00, temperature normal. Kim appears to feel better. Overnight temperature normal.
25 October 2011, Tuesday
Morning, temperature goes up to 38.1°C.
12:00, 38°C.
12:30, 38.5°C, called hospital, give Paracetamol.
14:00, ambulance arrives.
15:00, arrive at emergency hospital.
General blood OK, blood counts are OK, urine OK,..so why??
WBC 2.0
Neutrophils 1.0
HB 101
Plt 236
17:00, given 2gm ABX Tazocin
Panadol, temperature goes up to 39°C.
Transferred to ward.
24 October 2011, Monday
03:00, opens bowel first time after surgery, all good.
09:00, Surgeon checks on Kim and says she should be able to go home later afternoon.
11:30, Hickman dressing cleaned/replaced.
17:30, discharged from hospital
18:30, arrive home.
23 October 2011, Sunday
09:30, iv fluid down to 20ml/hr
10:30, morphine down to 05 ml/hr
17:15, morphine stopped
(other medications)
22 October 2011, Saturday
Kim slowly recovers from yesterday's surgery. She is drowsy but upbeat.
15:00, hurray she eats, 40ml of soup.
16:45, 120ml mix water and cranberry juice.
17:15-19:00, plays a little in bed and eats half a jelly.
21 October 2011, Friday
14:15-18:40 Laparoscopic Surgery removed the tumour and nodes near her artery. It was a clean removal and the tumour was taken out in one piece. Her kidney was pushed aside and partially encapsulated by the tumour but it seems it did not encroach into the kidney. The kidney could stay and a full recovery is expected. The surgeon inspected but did not find any nodes in pelvis area. The chemo has removed all the nodes. There were no complications.
20:00, Kim arrives at the ward.
She is given morphine (5.5mg/50ml 1ml/hr) and 40ml/hr Hartmann's solution through iv and seems to cope well.
20 October 2011, Thursday
11:25 met with Oncologist. Everything good and on track.
13:00, met with surgeon. Discussed laparoscopic surgery tomorrow. Signed consent forms.
Weight 10.45 kg
Height 82 cm
Neutrophils 0.5
Platelets 230
Urine test fine
Hickman dressing cleaned/replaced
17 October 2011, Monday
07:30, no more solid foods until CT (CAT) scan finished.
11:30, no drinking/fluids until CT (CAT) scan finished.
11:40, non-emergency ambulance to hospital.
16:40, CT (CAT) scan abdomen, pelvis, chest.
17:00, in recovery room.
from October 2011, missing dates
Why are some dates missing?
In October 2011 we were trying to get Kim's Oma (grandmother) to stay in Australia on a carer visa. Her care saved Kim. She made sure Kim ate healthy and got her to eat while we (parents) and nurses couldn't convince Kim to take a bite. Kim's grandmother has been helping caring for Kim since her birth and there is a strong bond between them. However, her one year family visitor visa came to an end. We were advised by the immigration lawyer to stop this website until the visa application was approved. Unfortunately Medibank (reviewing Kim's health for immigration) found that Kim did not qualify for her grandmother to get a carer visa. Reason being that Kim's condition and need for extra care was not stable for at least two years. A lot of discussions on what the immigration rules and conditions are, how they are, or should be, interpreted etc. But in the end a lot of time and money wasted. Immigration lawyers are very expensive (to be fair this one gave a discount).
Once Kim's grandmother was gone her appetite was indeed not as good. Her recovery times slowed down. But luckily Kim had the worst behind her and she pulled through.
14 October 2011, Friday
First night at home and Kim sleeps good.
13 October 2011, Thursday
Kim can go home as her bloods are getting better. She did not need another blood transfusion.
White Blood Cells 6.6
Haemoglobin 122
Platelets 30
Neutrophils 4.7
12 October 2011, Wednesday
Kim's temperature drops to 33°C in the middle of the (Tue/Wed) night.
Maybe another blood transfusion is needed tomorrow.
Weight 10.1 kg
White Blood Cells 1.7
Haemoglobin 111
Platelets 16
Neutrophils zero/none.
11 October 2011, Tuesday
04:00, Arrived at cancer ward from emergency.
04:15, Blood transfusion is given.
First blood test results show:
White Blood Cells 0.4
Neutrophils (none/zero)
Haemoglobin 68
All very low.
Fluids are given throughout the day. Oncologist says that Kim will stay for the next couple of days as she needs to be guarded with the low blood counts.
19:00, for her anal pain relief she is given an Morphine Sulphate Intrasite Gel and a Zinc Oxide Ointment.
21:20, Kim falls asleep late.
10 October 2011, Monday
Kim had a restless sleep last night with a lot of waking up and crying. Clearly she does not feel good. She felt a bit warm in the middle of the night, but soon stabilised.
12:00, Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF) at home by Mama.
Around 19:00 Kim her temperature increased again to 38°C. We see if it drops, first it does, but then it came back up to 38.5°C. We call the hospital and go.
Around 22:30 we arrive at hospital emergency. Bloods are taken and antibiotics are given.
Weight 10.3 kg
09 October 2011, Sunday
Kim did not have a great sleep, restless. By 10:00 she has a slight fever, 37.5°C. We consider the need to go to the hospital. She seems a bit out of it, but no specifics. Previously we would have called the hospital immediately as per their instructions. (call if fever, call and go if over 38°C) This time we don't as we know from experience that going through emergency with all the pricking and poking is very stressful on Kim. We keep a good eye on her temperature and an hour later it dropped to 36.5°C. Later in the day another slight fever peak of 37.8°C which soon dropped again.
Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF) at home by Mama.
Kim ate reasonable today, not great but OK. She is getting more and more difficult about food now. Part her illness I am sure, but also the fact that she is spoiled with getting whatever she wants due to us not wanting to upset her. If she gets upset it can trigger fevers, etc. In addition she needs all the food we can get in her. If her weight drops below 10 kg they may need to delay treatments.
Kim did not go out today as the weather changed. She also seems to look uncomfortable and with her fevers we wonder if this is caused by her trip outside yesterday. She is also sometimes pointing to her behind and we wonder if she has an anal fissure.
08 October 2011, Saturday
Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF) at home by Mama.
Kim, is difficult today and very active. She does not seem sick, but it is probable that she feels that way.
The weather was nice enough to go into the front garden with Kim where we spend a lot of time looking at the little airplanes flying over, cars driving by, people and dogs walking past. She says to each and everyone of these, "hello" and "bye bye".
07 October 2011, Friday
Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF) at home by Mama.
06 October 2011, Thursday
12:30, Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF) at home by Mama.
19:30, Kim feels bad and vomited. After she eats a little again before going to bed.
05 October 2011, Wednesday
12:30, Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF) at home by Mama.
04 October 2011, Tuesday
13:00, Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF) at home by Mama.
03 October 2011, Monday
Kim is doing OK. Better now that she is home.
02 October 2011, Sunday
Final day of fourth chemo cycle.
17:00 Kim can go home, arrive home 18:00.
Kim shows that she is not feeling 100%, but on the other hand is still happy and we don't notice any side effect like nausea etc so far. But that we don't notice doesn't mean she doesn't feel it. Anyway, she didn't throw up or became lethargic.
01 October 2011, Saturday
Third day of fourth chemo cycle.
Weight 10.52 kg, good, still going up.
Kim still eats good, but less than before. Probably due to the chemo. Tomorrow is her last chemo day and may go home by the evening.
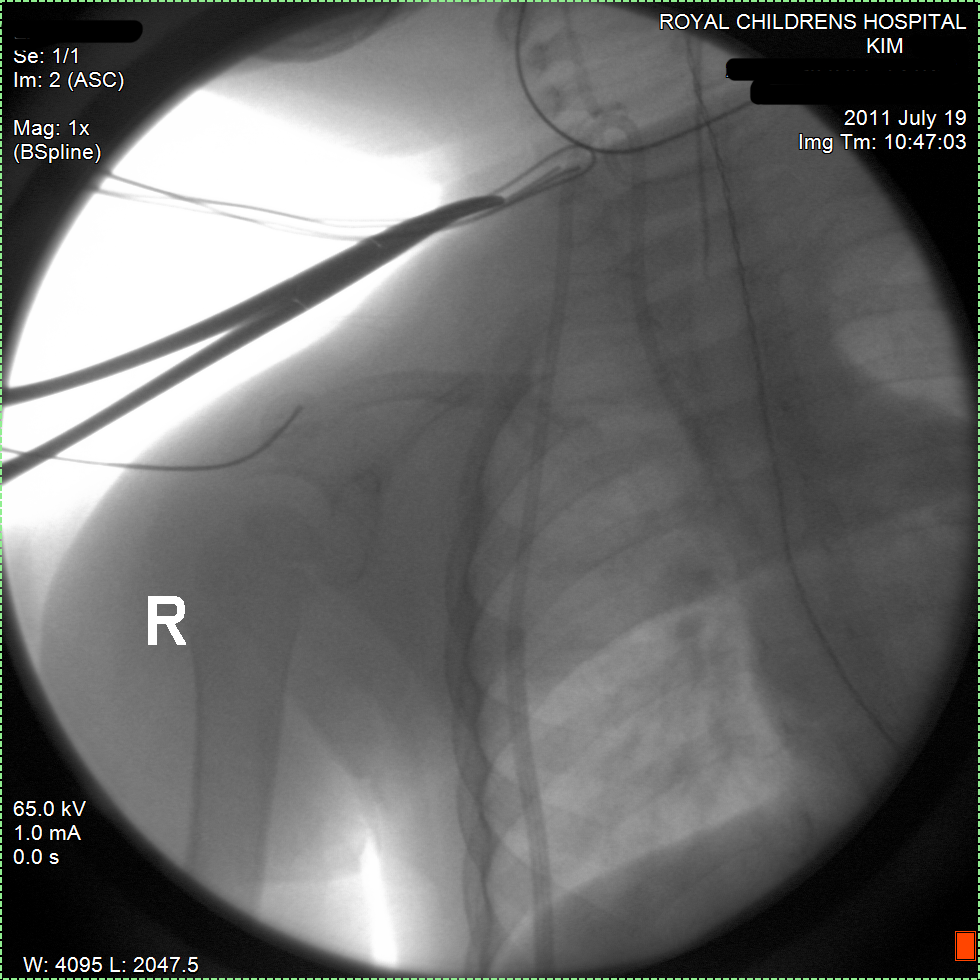
30 September 2011, Friday
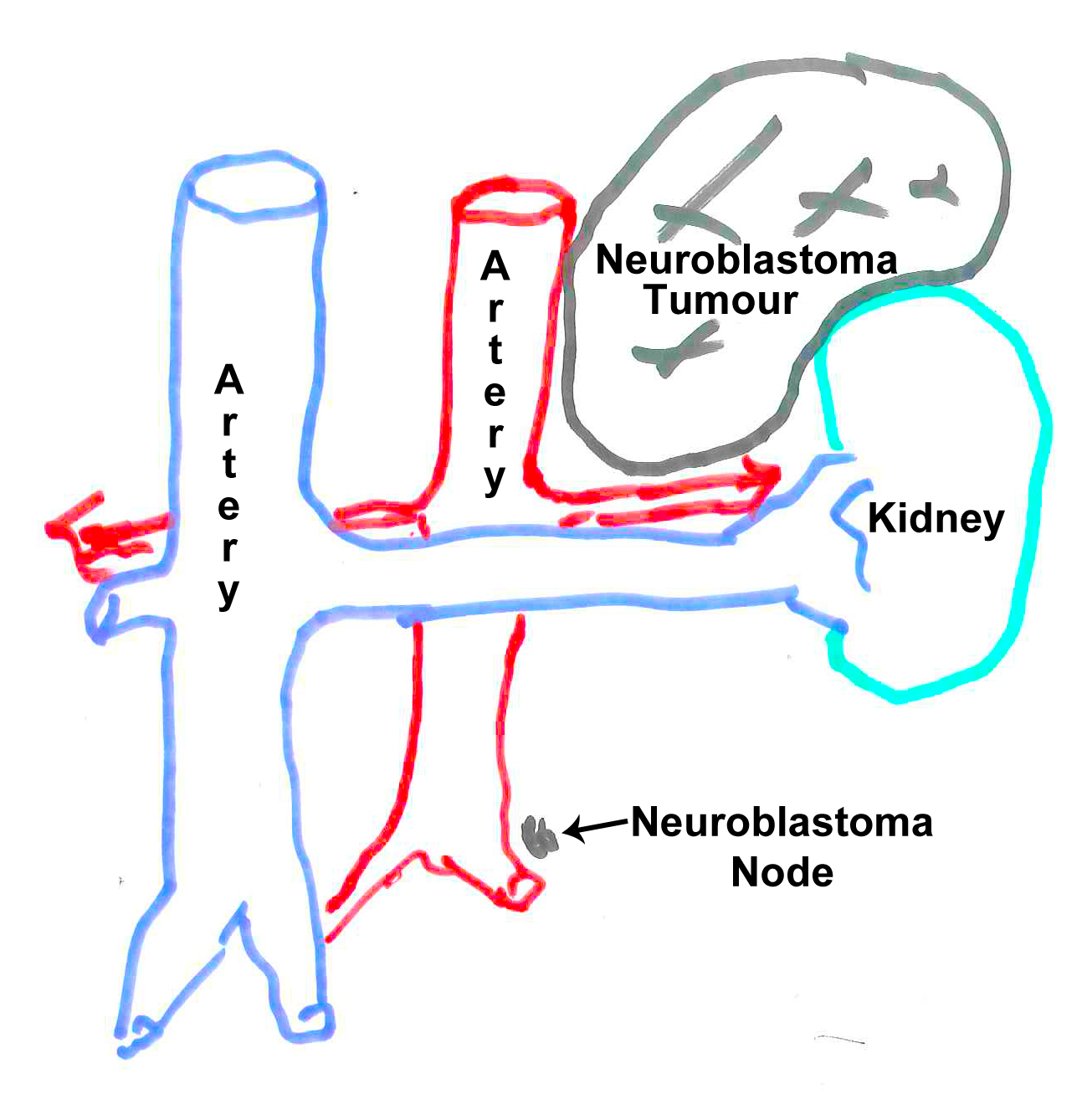
07:00, met with oncology surgeon who confirmed that surgery is set for 21 October 2011. He explained that he did not expect any complications and that he is very happy with Kim's progress. He drew the picture above to explain that the Neuroblastoma node is very small and may be gone at the time of surgery, although he will still investigate the area during surgery. He also explained that he did not expect that Kim will loose her kidney. The tumour is close but did not seem to invade the kidney so she probably will not loose any part of it. While previously the tumour seemed to get too close to the arteries, now it looks very good and it will be a straight forward procedure for the surgeon. The procedure will take around 4 hours. She is planned to stay in hospital for post surgery recovery for 4 days and will probably be down and in bed for the first two. The last two days she is expected to become her active self again. Then off to home and following with next Chemos etc. The surgery date will only change if her blood levels are not good because of the prior chemo and any side effects. But it is expected she will be OK. She has been doing good so far.
13:00, Renal specialist came to look at Kim. Kim's blood pressure seems to be more stable now. We can stop with Captropril, one of the three blood pressure medicines she is taking now.
Second day of fourth chemo cycle
21:30, Kim woke up crying badly. Not sure why, probably because of nausea. Carrying her around calmed her down.
23:30, Kim woke up crying badly. Not sure why, probably because of nausea. Carrying her around calmed her down.
29 September 2011, Thursday
Kim admitted for fourth Chemo cycle. This time the chemo is given non-stop for 24hrs for 3 days. Chemo started around 16:00/17:00.
28 September 2011, Wednesday
Kim is a very active and happy girl. When she sees food she will open her mouth wide open and point. We are all happy because of that. Kim has a very good appetite these days nearly non-stop eating
Weight 10.2 kg.
27 September 2011, Tuesday
Kim is earlier tired in the evening, but does not want to go sleep. She wants to stay awake to play with us.
26 September 2011, Monday
07:30, On the way to work papa drops Kim and mama off at the hospital for her blood tests, and possible blood transfusion.
09:00, Blood results are good:
Haemoglobin 100
Platelets 135
White Blood Cells 9.8
Neutrophils of 7.59
No need for blood transfusion and have to come back on Thursday for admission, next (4th) Chemo cycle.
11:00, arrive home.
It is a sunny day and Mama and Kim travel for the first time back home by public transport (tram and train). Nervous and afraid that she may pick up something from the other passengers.
25 September 2011, Sunday
Kim starts to nag more in the evening.
It is sunny and warm weather and we take Kim to her first outing in a long time. We spend approximately 45 minutes on a second hand market. Kim choose a new toy for herself. She did get a runny nose and was tearing.
24 September 2011, Saturday
10:00, Blood tests done at Day Oncology, papa brings them urgently to laboratory.
Blood results are still good enough:
Haemoglobin 88
Platelets 44
White Blood Cells 12.3
Neutrophils of 9.52
No need for blood transfusion and have to come back on Monday for further tests.
Weight 10.2 kg with clothes on, a slight increase but better than loosing more weight.
23 September 2011, Friday
Papa takes off from work to bring Kim to the hospital for new blood tests and possible transfusion. Halfway there he gets a call that Kim can come in tomorrow (Saturday) and may need to stay then for blood transfusion.
22 September 2011, Thursday
10:50 bloods taken by Nurse at Home service.
11:40, injection under the skin of Granulocyte Colony Stimulating Factor (GCSF) by Mama.
16:00, we get a call from the hospital that the bloods arrive at the laboratory in a clotted state. This is the third time this happens. It is really frustrating as the Nurses at Home (an agency contracted by the hospital) always work messy and don't seem to be able to take the bloods right. Now Kim has to go to the hospital to do the bloods there. Oncologists does not like Kim travelling too often/much, and neither do we.
21 September 2011, Wednesday
11:40, injection under the skin of Granulocyte Colony Stimulating Factor (GCSF) by Mama.
Kim is eating better.
20 September 2011, Tuesday
08:00, Kim eats good pick nick breakfast while in the hospital.
08:00, bloods are taken in Day Oncology. Papa brings bloods to lab on 2nd floor, marked urgent. (for 09:00 appointment)
09:00, appointment with oncologist delayed until 10:00.
Length 82.2 cm
Weight 9.7 kg
Blood Pressure (BP) 83/45 (first reading 140/70, electronic BP equipment always has different results.)
Blood results are good:
Haemoglobin 92
Platelets 85
White Blood Cells 8.7
Neutrophils of 7.1
10:00, Oncologist is overall happy with progress. A Worry is Kim's weight loss. She needs to stay above 10 kg for the chemotherapies. If she balances at this weight or drops further she may need to be fed through a nose-tube. It is expected that Kim may need a blood transfusion later this week.
Oncologists explains that previous comment by her colleague stating that Kim may not need the full heavy chemo cycle is not correct. Except for timing of surgery and chemo start dates the treatment plan will normally not be altered.
11:00, injection under the skin of Granulocyte Colony Stimulating Factor (GCSF) in hospital.
13:00, return home.
19 September 2011, Monday
Kim eats good, breakfast and lunch.
11:40, injection under the skin of Granulocyte Colony Stimulating Factor (GCSF) by Mama.
16:00, Kim vomits, just a little.
Kim eats good dinner.
18 September 2011, Sunday
Kim breakfast and lunch are reasonable and promising.
11:40, injection under the skin of Granulocyte Colony Stimulating Factor (GCSF) by Mama.
Kim eats good dinner, may be too much too quickly.
21:00 Kim vomits in bed.
17 September 2011, Saturday
11:30, injection under the skin of Granulocyte Colony Stimulating Factor (GCSF) by Mama.
Kim has lost a lot of weight. We did not check the weight yet but it is obvious. Thinner thighs, legs, etc.
16 September 2011, Friday
14:00 Hickman dressing change and injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
Kim seems to eat a little better, but not much at all and she is a bit lethargic.
16:50 Kim vomits
15 September 2011, Thursday
Kim eats little.
13:00, at home, injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
Papa is away for work to Sydney. There he meets by coincidence with the CEO of the Cancer Council of Australia. In a hallway we discuss a few minutes the Cancer Council's view on, and dealings with, Neuroblastoma. The CEO confirms that paediatric research into cancers are pretty good and outside the scope of the Council. The Council does not really do much in the paediatric area as it does not seem to need extra help. The Council mostly focuses on cancers with a lot of public and media attention where they feel there is a need for further help. Maybe I don't write it all down correctly here, but this is how I remember the conversation. And although the CEO was a nice and sympathising person it gave me the impression that unless there is a lot of public attention on a cancer/issue not much is done. Although that was not directly said by the CEO.
14 September 2011, Wednesday
11:30, at home, injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
Kim vomited, not much as she probably has little stomach contents..
13 September 2011, Tuesday
13:30, at home, injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
Appetite is not good.
12 September 2011, Monday
Kim vomited twice, morning and afternoon. She does not really eat.
15:45, Kim is discharged from hospital.
11 September 2011, Sunday
09:30, vomited
Weight 10.04 kg
16:05, 4th Chemo and final course of 3rd cycle.
Kim eats very little.
10 September 2011, Saturday
14:45, 3rd Chemo course of 3rd cycle.
Weight 10.04 kg
15:00/19:40, Chemo has strong effects on Kim, she throws up twice.
Kim is not really eating well.
09 September 2011, Friday
14:45, 2nd Chemo course of 3rd cycle.
Weight 10.6 kg
20:30/21:00, Chemo has strong effects on Kim, she throws up twice.
Loss of appetite.
08 September 2011, Thursday
Red Cross pick up for transport to hospital.
15:10, 1st Chemo course of 3rd cycle.
Neutrophils 6.92 weight 10.4kg, bloods OK
07 September 2011, Wednesday
OK day
06 September 2011, Tuesday
OK day
05 September 2011, Monday
11:30, at home, injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
13:30 Mama removed canula
04 September 2011, Sunday
10:00, at home, injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
03 September 2011, Saturday
09:00, we have been given 100 mg GCSF syringes but suspect this should only be 50 mg as stem cell harvesting has finished. We call the hospital and the nurse in charge says to give her 100 mg injections for the next three days. We also discussed her throwing up and loose stool. We are advised to watch it but it is probably due to side effects from one of the many medicines she is getting. It is unlikely to be due to (higher dose) GCSF.
10:15, Kim has watery loose stool (diarrhoea) yellowish in colour.
11:15, at home, injection under the skin of Granulocyte Colony Stimulating Factor (GCSF). Nurse says order is only for 50 mg. He phones with hospital and nurse confirms only 50 mg to be given. Half a 100 mg dose is given. Temperature 35.9°C but nurse (Peter) says it is probably a little higher as his ear thermometer did not have good access to ear.
Kim is a little less energetic but seems very happy to be home. She loves to walk and stretch her legs, although a little unstable on her feet after lying in the hospital bed for so long.
02 September 2011, Friday
10:30 catheter connected to harvest stem cells machine.
Molly, one of the Fellows mentions that Kim may not need the full high dose Chemo therapy (Maintenance Therapy). This is great news, but Consultant needs to confirm this. Consultant later explains this is not correct, see 20 Sep 2011.
White Blood Cells 2.1, stem cell harvesting will start.
Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
14:52 stem cell harvesting is finished. In 262 minutes 219 ml of blood collected with stem cells. The laboratory will check if enough is collected.
approx 16:30 laboratory confirms results:
We needed more than 2.54 x 106 / kg. Laboratory confirms nearly 12 x 106 / kg is collected, more than enough. Good, so she doesn't need to do this again.
17:00 catheter is removed. Kim has to lay flat until 21:00, after can be discharged.
21:00, discharged and going home. Kim will start her 3rd Chemo Thursday 08 Sep 2011.
22:30 Kim coughs in her sleep and this triggers her to vomit. Full stomach contents.
01 September 2011, Thursday
06:00, CD 34, White Blood Cells 1.0
18:30, Kim has watery loose stool (diarrhoea) yellow-green colour
Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
Kim has loose stool (diarrhoea) 3x, green colour
Stem cell harvesting delayed till tomorrow.31 August 2011, Wednesday
06:00, CD 34, White Blood Cells 0.5
Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
13:50 given Midazolam 6 mg to relax for surgery (Femoral catheter insertion)
14:10 Anaesthetic given and Femoral catheter surgically inserted.
15:05 Kim comes back to surgery recovery room and starts to wake up.
15:45 back to the ward with a few more tubes going into her body.
Hopefully her blood levels will come up tomorrow so she can get the stem cell harvesting done.
30 August 2011, Tuesday
06:00, CD 34, White Blood Cells 0.2
Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
Kim's stem cell harvesting is delayed. She fasts from midnight for Femoral catheter surgery (special catheter for stem cell harvesting).
Kim has slightly loose stool (diarrhoea) 3x, green colour, a stool sample was taken.
29 August 2011, Monday
08:00, injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
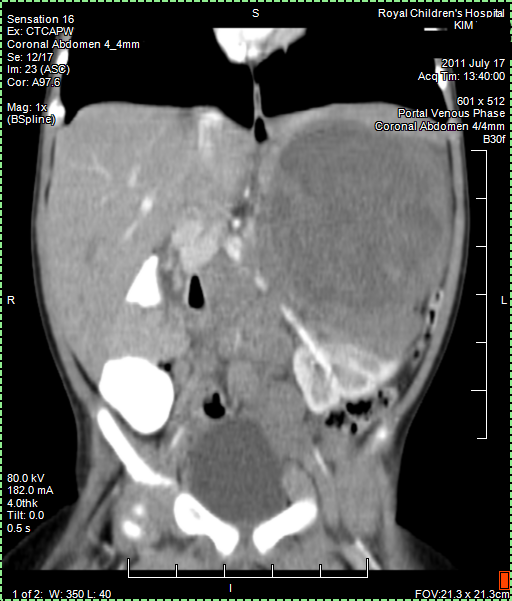
Today we got the Radiology Report back of the 25 August CT (CAT) scan. Papa still has a few remaining questions about it but it confirmed that the tumour shrank as papa thought to see himself from the images. Good news!
Kim's stem cell harvesting is delayed. Maybe tomorrow. She fasts from midnight for Femoral catheter surgery (special catheter for stem cell harvesting).
Weight 10.7 kg, White Blood Cells 0.3, CD 34
28 August 2011, Sunday
09:00, at home, injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
10:30/11:30, Kim becomes irritable and also seems tired. Temperature 37°C
15:20, arrive Emergency temperature 39.5°C
Later temperature goes up to 38.5°C. We are advised to go to Emergency. Kim was due to be admitted tonight for Stem Cell harvesting Mon-Wed.
15:50, antibiotics are given through IV, plus several bloods taken for cultures etc. First results show Haemoglobin at 81, Neutrophils 0.2.
approx 17:00, admitted to Oncology ward. We are told tomorrow will continue as planned if bloods are OK at the time. Blood transfusion given to increase Haemoglobin.
approx 22:45, bloods taken for more tests.27 August 2011, Saturday
08:50, at home, injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
Temp 36.5°C
Happy and playful
26 August 2011, Friday
08:15 blood finger prick taken at Day Oncology in preparation for Oncologist meeting.
09:45 Meeting with oncologist. No results back yet from CT (CAT) scan. Weight 10.54kg and length about 81cm nurse was not very focused on checking length.
10:30 More blood taken through Hickman for further tests in preparation of Stem Cell Harvesting on Mon-Wed. Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF) was given at around the same time. Neutrophils 0.3.

Papa collected copy of CT (CAT) scan images from Radiology. Looking at them it seems that the main tumour shrank from around 11 cm to 6 cm and there is less evidence of Nodes. But we have to await Radiology Report to be sure about this positive news. Lets hope Papa is right.
Blood test results of today show her White Blood Cells are down (expected just after Chemo).
Asked pharmacy about possibility of giving Kim herbal medicines such as Reishi Mushroom (Ganoderma Lucidum). Pharmacy gave us some print outs with further information. We have to be careful considering this.
25 August 2011, Thursday
Kim had to fast from 07:00 in the morning so she was given a very early breakfast. Later this afternoon the CT (CAT) scan.
16:10, CT (CAT) scan under general anaesthetic. Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF) was given at the same time. When Kim woke up she was not very happy and all in all it was a grumpy day. We hope that results will come back quickly, tomorrow?

Weight 10.56kg, all other obs normal.
24 August 2011, Wednesday
14:10, at home, injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
Kim is happy. She likes to build with large Lego blocks. Improving on her hand/eye coordination. And she likes lots of cuddling. She is very picky about food these days and still does not have her usual appetite back. Her fluid intake is poor these days (she drinks very little).
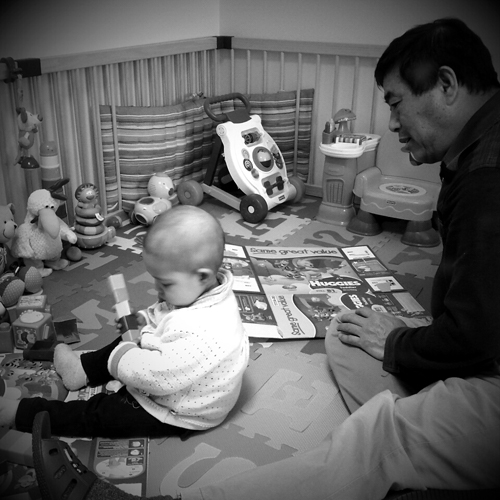
Kim playing with Opa ("Opa" is Dutch for grandfather)
23 August 2011, Tuesday
14:20, at home, injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
Happy and playful
22 August 2011, Monday
13:20, 5th Chemo course of 2nd cycle (last one for this cycle)
Weight 10.44kg and all other obs good.
Nutritionist mentions how Kim is doing well. Most kids in her situation don't eat and lose weight and have to be fed through a tube through the nose.
It tells us again how important her eating is. Kim eats very well with her Oma (Grandmother) and if it wasn't for Oma Du her condition and situation would probably be much worse. Oma has been there supporting us most of the time and never leaves Kim.
17:30, Kim is discharged (can go home). She will have to come back on Thursday for CAT scan (CT) and on Friday Oncologists wants to see her for the planned Bone Marrow Stem Cell harvesting on Monday.
21 August 2011, Sunday
Kim seems to be constipated. Weight 10.45kg all other obs are good.
Appetite remains poor, this is expected with the Chemo.
13:00, 4th Chemo course of 2nd cycle
Blood tests all OK
20 August 2011, Saturday
13:00, 3rd Chemo course of 2nd cycle
Loss of appetite in the afternoon.
Blood tests all OK
19 August 2011, Friday
08:00, Kim has slightly high blood pressure.
14:20, 2nd Chemo course of 2nd cycle
18 August 2011, Thursday
09:00, Kim gets blood test in the morning followed by Oncologist appointment. Her Neutrophils are back up to 1.3. Although still has flue, this is OK for Kim to start 2nd Chemo therapy today. Weight 10.75kg. Normal temperature.
13:45, Kim has a hospital dentistry check up.
15:00, Kim finally starts 2nd Chemo.
Cyclophosphamide (CPM) IV over 30-60 minutes
13.3 mg/kg/dose daily for five daysTopotecan (TOPO) IV over 30 minutes
1.2 mg/m2/dose daily for five days
She is very active and happy in the hospital and tires Mama and Oma ("Oma" is Dutch for Grandmother) out.
17 August 2011, Wednesday
Blood taken at home. Again, by the time it reaches laboratory it has clotted and can't be used anymore. Another test tomorrow morning. Normal temperature.
16 August 2011, Tuesday
Kim sneezes sometimes. She is happy and eats good.
15 August 2011, Monday
Weight 10.5kg, blood tests and NPA which showed Influenza A. Neutrophils are low at 0.5. Kim can not start 2nd Chemo until her Neutrophils are back up.
14 August 2011, Sunday
Normal temperature. Kim has better appetite for vegetables and chicken. Here eating improves every day.
13 August 2011, Saturday
Slight dry cough, normal temperature. A happy day for Kim.
12 August 2011, Friday
Normal temperature. A happy day for her with smiles and laughing.
11 August 2011, Thursday
03:00, Kim's temperature drops to 36.5°C and stabilizes. The night is spent in Emergency.
09:30, meeting with Oncologist. All bloods are good, but need to check snot for possible flue. Kim has no runny nose, so a tube is inserted into her nose to gather snot (NPA) for pathology. Kim was supposed to start 2nd cycle Chemo today but this will have to be delayed until all tests results are back clear. Hickman dressing is cleaned and changed. New appointment is made for tomorrow and Kim is sent home.
16:00, Hospital called to confirm that Kim has the flue. Appointment tomorrow is cancelled and she needs to come back on Monday to see if Flue is gone (again blood and NPA). Then maybe can start 2nd cycle Chemo. (Delaying Chemo is not good, lets hope this is the first and last time). Papa feels very bad as he got the flue first.
10 August 2011, Wednesday
10:30, community nurse collects blood and takes temperature, 36.5°C
Photo at emergency, also shows her hair loss.
18:30, Kim has a red flushed face and a temperature of 38.6°C. We have to go to Emergency where Kim is admitted. Temperature goes up to 39°C. Further blood tests are taken. Neutrophils are good, up to 4.02.
09 August 2011, Tuesday
Nothing to report.
08 August 2011, Monday
Kim starts walking a little. Again a happy day.
During night wakes up quite a few time crying.
07 August 2011, Sunday
Kim is getting more vocal and playful. Papa got a cold and is banished to the bedroom. Any cold she gets can become a big issue and lead to fatal complications. At best it would delay treatments and that could mean higher chances for the cancer to become resistant or grow back. Any delay is therefore also not good at all.
Papa normally beliefs that having a cold needs to be overcome by the body itself and medications should be avoided. This way your own resistance stays strong. However, now the situation is of course very different. Papa takes medication to minimize exposing Kim.
06 August 2011, Saturday
Kim eats good. Mama made some pictures while Kim still has most of her hair. Her first treatment of Chemo seems to be effective. Although we have no scans or anything to proof that now, we see here smiling more, being happy again.
05 August 2011, Friday
Kim starts crawling around. She hasn't walked for some time now.
Kim starts to loose a lot of hair.
Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
04 August 2011, Thursday
Outpatient appointment with oncologist.
Weight 10.5kg
length 80.9cm
Neutrophils 0.8.
She is doing well in recovering from 1st Chemo.
Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
03 August 2011, Wednesday
Eating improves every day. More smiles.
Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
02 August 2011, Tuesday
Bone scan results not clear, poor uptake of contrast material. Some evidence above the left knee. Which matches earlier CT.
Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
Kim sleeps well.
01 August 2011, Monday
Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
Blood tests show Neutrophils at 0.06. This is expected, but it puts her at risk. A healthy child would have Neutrophils anywhere in between from 1.0 to 8.5.
10:45, Bone scan
13:00, 2nd Bone scan
Swab Hickman is clear
(the Hickman are the tubes going into her body. These need to be kept very clean and swabs are tests to check if there are any bacteria etc.)
Kim is released and can go home for a break.
Medications have high blood pressure under control.
31 July 2011, Sunday
Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
Medications stabilizes high blood pressure
30 July 2011, Saturday
Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
Medications stabilizes high blood pressure
29 July 2011, Friday
Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
A number of medications stabilizes her high blood pressure
28 July 2011, Thursday
Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF)
mIBG scan results not very clear due to poor uptake of contrast material. Some spots on her left leg, not sure if correct. "Could be pee on her leg with contrast material" (unlikely she was clean, see Bone scan results 02 August 2011).
High blood pressure up and down
27 July 2011, Wednesday
Injection under the skin of Granulocyte Colony Stimulating Factor (GCSF). This stimulates the production of Neutrophils. Neutrophils are types of white blood cells and an essential part of the immune system. Without sufficient Neutrophils the body is not able to fight colds and other diseases. A little cold could become a huge risk.
11:45, mIBG whole body scan
High blood pressure up and down

26 July 2011, Tuesday
10:50, 5th dose of 1st chemo cycle
11:30, injection of contrast fluid for mIBG scan.
15:30, abdomen mIBG scan.

Appetite reasonable
Weight 10.4 kg, high blood pressure
25 July 2011, Monday
Eating improves
Kim enjoys the ward's playroom with toys (was closed during the weekend). She does not want to walk and it looks painful. She does not crawl and sits on mat or children's chair.
10:50, 4th dose of 1st chemo cycle
High blood pressure
24 July 2011, Sunday
11:20, 3rd dose of 1st chemo cycle
16:00, vomited
18:00, temperature 38°C
High blood pressure
23 July 2011, Saturday
Temperature 38.2°C
11:00, 2nd dose of 1st chemotherapy cycle
13:00, vomited
High blood pressure
22 July 2011, Friday
110 ml blood transfusion
1st bath after Hickman insertion/surgery.
08:30, Kim is Transferred to CCC ward.
11:00, Kim receives 1st dose of 1st chemotherapy cycle
Cyclophosphamide (CPM) IV over 30-60 minutes
13.3 mg/kg/dose daily for five daysTopotecan (TOPO) IV over 30 minutes
1.2 mg/m2/dose daily for five days
High blood pressure
21 July 2011, Thursday
After six days in the hospital we are told the results are back in. The oncology team wants to meet with us (parents) in a meeting room (13:50) on the surgical ward. They confirm it is Neuroblastoma MYCN amplification stage 4, an aggressive form of this child cancer. We know it is the worst type there is. We are sitting around a table and the team is very business like, straight forward. It was very tough to hear this and we are of course very emotional. But the straight forward approach is also sobering and gives us the strength to focus on what we can do, what next to fight this. The language is carefully chosen, not mentioning the worst case scenarios, not mentioning the chances, but focusing on what can be done. (Only days later mama accepts the real threats, until then she tries to ignore the severity).
An intensive treatment is required and there is a (high) possibility of relapse. The "situation is serious". We can expect to spend more time in the hospital than at home over the coming year. The treatment plan is given to us. But we are very emotional and find it difficult to concentrate on the details. We are assured that we won't find more up to date treatment elsewhere in the world. We are in the best possible place for Kim to have the best chances. We ask that the chemotherapy starts asap.
During our meeting Kim went to a hearing function check. This is done before the chemo in order to see later if her hearing will be affected by the chemos (hearing loss is one of the side effects).
Kim receives hydration through IV. Around 17:00 we hear that pharmacy did not release the chemotherapy due to Kim being on the surgical ward instead of the Cancer Centre ward. We are told that Kim requires hydration for 12 hours anyway. (later we read in the treatment plan this is 2 hours before and after each dose).
High blood pressure
20 July 2011, Wednesday
15:00-16:00, temperature over 38°C
Treatment will need to wait until all tests results are back from Pathology. We are advised that Chemo can be started on surgical ward by Cancer Centre nurses.
First test results confirms Neuroblastoma, but which type/stage?
High blood pressure
19 July 2011, Tuesday
Evening, her fever goes over 38°C
Biopsy of mass, bone marrow aspiration and Hickman catheter surgery. Finally done, but now the samples are going to Pathology (laboratory).
High blood pressure
18 July 2011, Monday
Fasted for surgical biopsy of mass and bone marrow aspiration (taken samples of the cancer and her bone marrow).
Also a Hickman catheter will be surgically implanted. These are tubes that will be put directly into her veins. Through these tubes chemo and medication can be given.
This was cancelled due to other children with emergencies. It's frustrating to think that there are just not enough theatres to handle all urgent cases.
High blood pressure

17 July 2011, Sunday
CT (CAT scan) abdomen under anaesthetic, confirms cancer. We await the Radiology Report. There is no way knowing what kind of cancer, but it is suspected maybe Neuroblastoma. We learn that there are different types of Neuroblastoma some of which are low risk and can easily be treated or removed. It is very worrying not knowing more.
High blood pressure
16 July 2011, Saturday
Kim had a limp and now in the hospital she is carried all the time, she does not walk anymore. (Only later do we learn that she had cancer nodes there and that the cancer grew quickly.)
Kim fasted for a CT (CAT scan) abdomen, under anaesthetic. This was cancelled, no availability due to other emergency priorities
150 ml blood transfusion
02:00hrs Transferred to surgical ward

15 July 2011, Friday
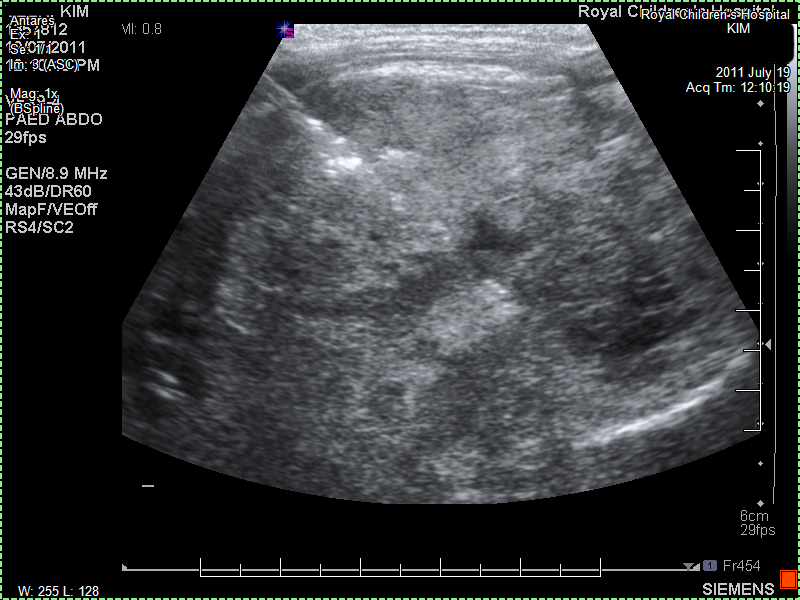
The paediatrician feels with her hands something in Kim's tummy. She gives us a gentle warning that there may be something there and refers us to a local imaging laboratory. She phones and makes sure we can be seen that same day. In the laboratory they ask us to wait. They tell us that there is an undefined mass near her left kidney. They don't want to say more. Ultrasounds are not that precise and we should go immediately back to the paediatrician. The paediatrician sees us almost immediately and tells us that it is not yet clear what Kim has but that it could be serious. At the same time she tries to comfort us with the knowledge that these days there are many new treatments. She doesn't want to use the word cancer but it is almost implied. She tells us she will refer us to the hospital to find out what it is exactly. The Monash is closer to us, but seen our previous experiences we ask to be referred to the Royal Children's Hospital. We insist that we have no trust in the Monash and will go to the Royal Children's. Which is traffic wise just a little further. The paediatrician mentions the close cooperation and that care should be the same. We are not convinced and the paediatrician is recognizes our resolve and understands why. She refers us to the Royal Children's Hospital emergency department with suspected cancer.
Thank god we did insist, looking back now it is best to go for the best. Don't hesitate to ask for the best, or travel a bit further for the best. It is certainly worth it. (and another tip is to have private insurance at the time your child is born and include her immediately). Of course, where there is an actual emergency and every minute counts, go to your nearest hospital emergency department. But if you can spend a little more on travel, then go for what you feel is best for your child.
Another thing I find amazing is that this paediatrician knew by touch that there was something wrong, and I could see the suspicion in her eyes. Why do not more doctors and GPs use those skills, I do hope they are still being taught!?
Later the Paediatrician writes to our GP and notes that "Kim has been unwell for about 4 weeks with non-specific symptoms of high fevers (up to 39.9), lethargy and poor appetite. She seems unsteady when she walks. No diarrhoea or vomiting.
Blood examination of 11 July 2011 showed a haemoglobin of 62 g/L and MCV of 73 fL (normal). Kim's diet is varied and when she is well she has a good appetite. On examination Kim was pale and had small axillary lymph nodes. The ENT examination was normal. She was not in cardiac failure. Her work of breathing was not increased, and she had a clear chest. Kim's abdomen was slightly distended, and she had an ill defined mass on the left side. She did not have hepatomegaly. She appeared slightly unsteady on walking, but she had a full range of movement of her hips, knees and ankles.
I have arranged an ultrasound scan of Kim's abdomen which shows a left sided mass, thought to be arising from her left kidney."
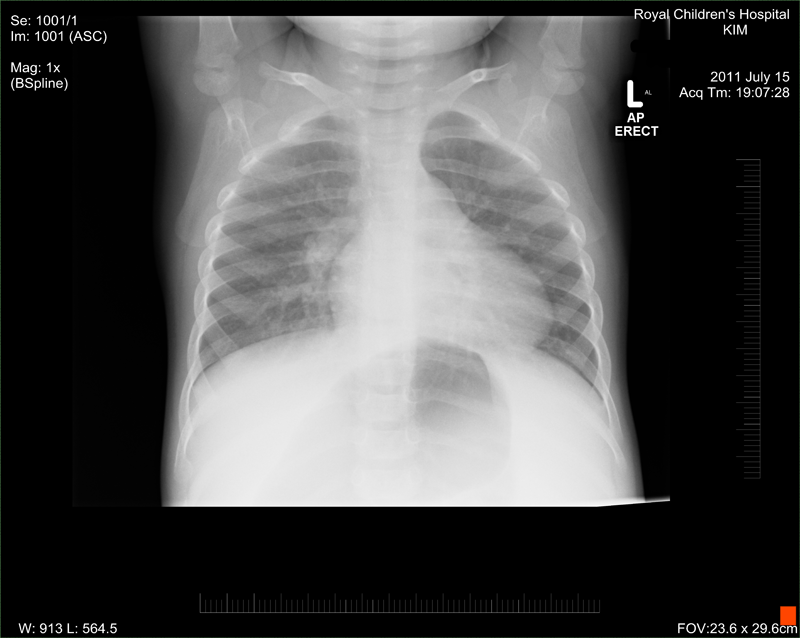
Emergency Royal Children's Hospital emergency organise an X-ray and some blood tests etc. The X-ray confirms a mass but it is not clear what it is, it only tells that there is something wrong. Later they organise her to be admitted. (We didn't know it but from that day on the hospital was becoming our new home.)
Before Diagnosis, 15 July 2011, Friday
This is written with hindsight...
At the time we have no idea what Kim had. We thought initially it was a cold. But the symptoms didn't really make sense. Kim was having intermittent fevers, roughly in the morning and afternoon, then a few days nothing, which gave us hope she was recovering from whatever she had. She was more lethargic, loss of appetite and poor fluid intake. Getting pale and just overall miserable. Only at the last few days showed minimal signs of a limp with left leg. She objected more and more to diaper changes and cried more. Her lethargic behaviour and crying was very unlike her. She was at an age where she just started speaking a few words, so she can't really verbally express what is wrong.
We did go to Monash Hospital which is in our area and has (had) a good name for paediatric care. The RCH do share some of their services and doctors with the Monash. However, we were there a couple of times at emergency and each time they sent us away. The doctors suspected that she had a cold and that was it. We requested blood tests etc but that wasn't thought necessary. More or less it was said that the hospital would not be able to cope if every child with a cold wanted a blood test. To be fair, initially she probably did have a cold and that didn't help things. But after the cold was gone and we came again to emergency and insisted on further testing we were told that she probably had another cold. We could not convince them to do further testing. We finally got an appointment with a GP. This wasn't easy as we just moved into the area and most GPs were fully booked for the next couple of weeks. The GP initially also did not see the necessity for further testing, however he was willing to listen to us parents and our wishes. So he referred us to do some further (in his mind unnecessary) testing. The blood results came back showing some abnormality upon which the GP referred us to a paediatrician who by coincidence was starting in the same medical centre that Friday (see above).
At the time cancer and Neuroblastoma was of course far from anyone's mind. Yes, it exists and does occur. But the percentages are so low that most Doctors never get to diagnose or see a case. Out of sight, out of mind! This makes it more unlikely for Doctors/GPs to recognize the possibility in the symptoms. We appreciate that being the case, but it should not be the case. There should be enough training and information out there for a GP/Doctor to want to look further and not just think it is another cold. Yes, colds can mask things, but it is also easy to say, "ah it is just a cold" and then wait and see. If symptoms are prolonged and are a bit off the norm, then do further testing. As parents we feel lucky that we persisted. By all accounts Kim came in at a time when she was nutritionally strong. We see a lot of kids who come in after they have lost a lot of weight and are very weak. Luckily Kim was not like that. These unfortunate kids have less strength to fight the side effects of chemo. They have many more risks, and sometimes (I don't want to look at the percentages) don't make it and pass away. We feel that if our experience reflects what is happening out there, a lot of kids are ignored until it is too late. The percentages that your child may have cancer is maybe low, but early detection can make a huge difference.

The above picture shows Kim some time before being diagnosed with cancer. At about one year of age we cut/shaved her baby hair off, sort of a custom. Her short hair in the photo has nothing to do with the cancer diagnosed later.